Get a true growth partner, not just outsourced medical billing
In-house billing teams fall behind as your practice gets busier. Generalist RCM services can’t keep up with the fast-moving changes that make dermatology so complex.

Clarity RCM offers the partnership, expertise, and scalability dermatologists need to build profitable, efficient practices at every stage of growth.
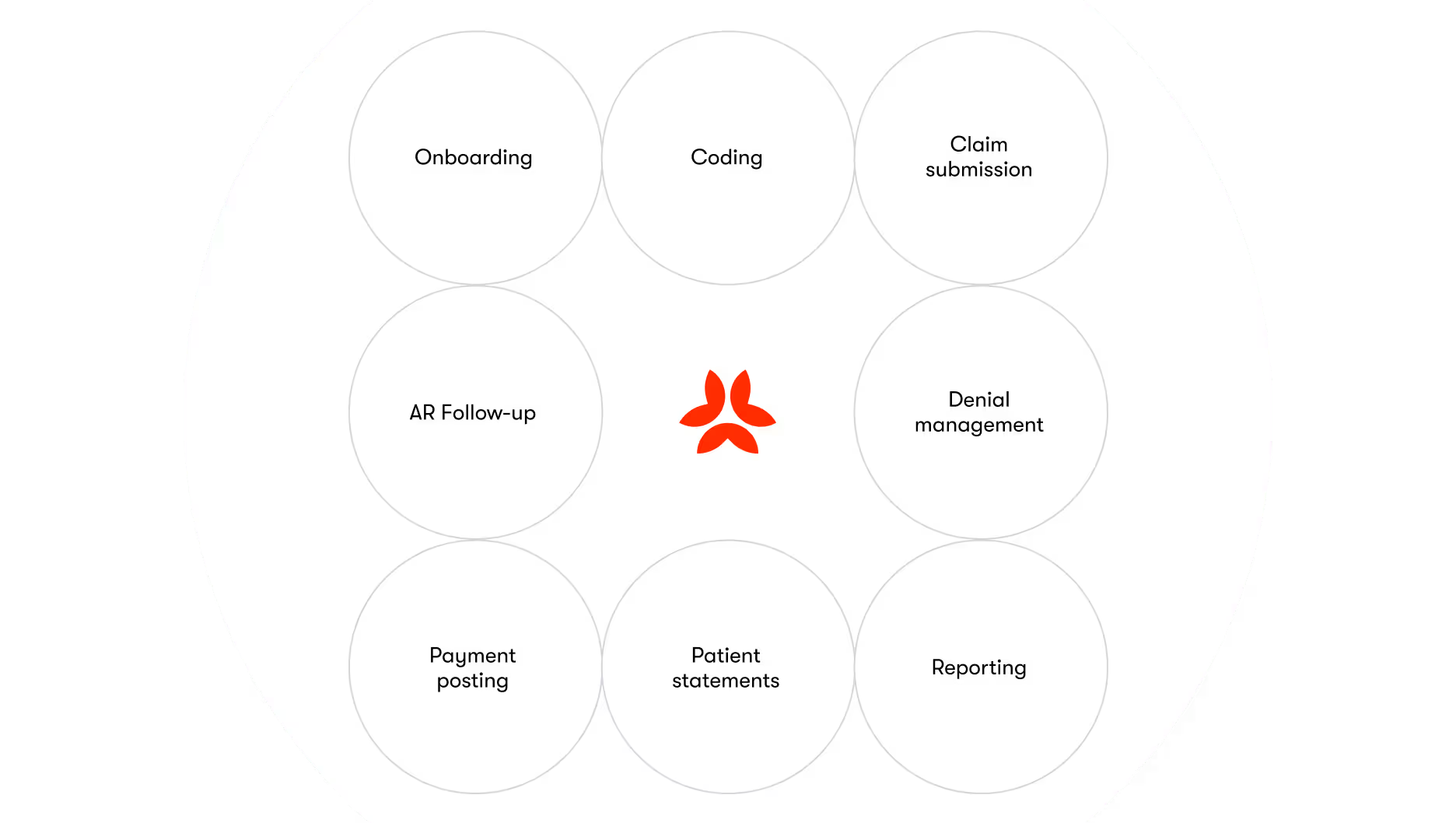
Our core RCM offering drives efficiency and results at every step in the process and avoids the pitfalls that hurt your revenue and slow down your growth.
Onboarding
Your account manager guides you through the transition, keeps you fully informed, and does all the heavy lifting. We can handle any changeover—from an in-house team or a third party—and work with any common billing software and electronic medical records platform.
Coding and documentation
Because dermatology is all we do, we get coding done right. We constantly optimize our process based on the latest coding guidance and denial trends, and we’re always available to meet, show you what’s happening, and educate you on what’s new.
Claim submission
We submit all claims daily and maintain a 98% clean claim ratio across all our clients. We monitor and manage charge entry performance indicators like days to enter charges, missing charges, and coding accuracy. We custom-configure your software to support scrub rules and add new procedures.
Accounts receivable follow-up
If a claim needs more work to be paid, we proactively investigate, find the root cause, and resolve it. We handle even the most complex, detailed claims. And we always analyze each case to understand how to stop the problem from happening again.
Payment posting
We ensure every payment is posted—no matter where it comes from or how it’s delivered. We handle all forms of payment from insurers and patients, including everything from in-office credit card swipes to mailed checks to EFT and ERA transfers to payments from your website.
Denial management
Strong denial management is a powerful defense against aged AR and lost revenue. Preventing denials in the first place is even better. With Clarity RCM, you get both. We handle the entire process, including appeals, and share learnings to mitigate preventable denials in the future.
Patient statements
We take ownership of your patient statements cycle, from manually checking each statement to posting payment and ensuring all payments are properly allocated. Deliver statements however you prefer: email, text message, or paper. We’ll manage cards on file, audit patient balances, and guide you through the process of capturing patient payments.
Reporting
Our custom reports and analytics summarize the health of your revenue cycle, identify opportunities for improvement, and offer granular detail when you need it. We’ll show you everything from AR trends to productivity reports to payer-specific trends to help you understand and improve your business.
We offer even more services than we can list here. Get in touch to learn all the ways we can help you get revenue under control.

We have friendly patient services reps located throughout the US, ready to handle every question your patients have about their bills. We’ll help patients understand charges, pay their bill, clear up any confusion about insurance processing, set up payment plans, and direct them to the right staff member in your office for more information when necessary.

Most payers need at least 90 days to credential a provider. That means credentialing can have a big impact on your revenue as you grow, add more providers, and expand to new locations.
We work with your team and payers to make sure that every clinician is fully credentialed, all credentials are current, and every credential-related issue is resolved. We handle the entire credentialing process, from information-gathering to submitting applications and storing credentials manually or with your preferred software program.
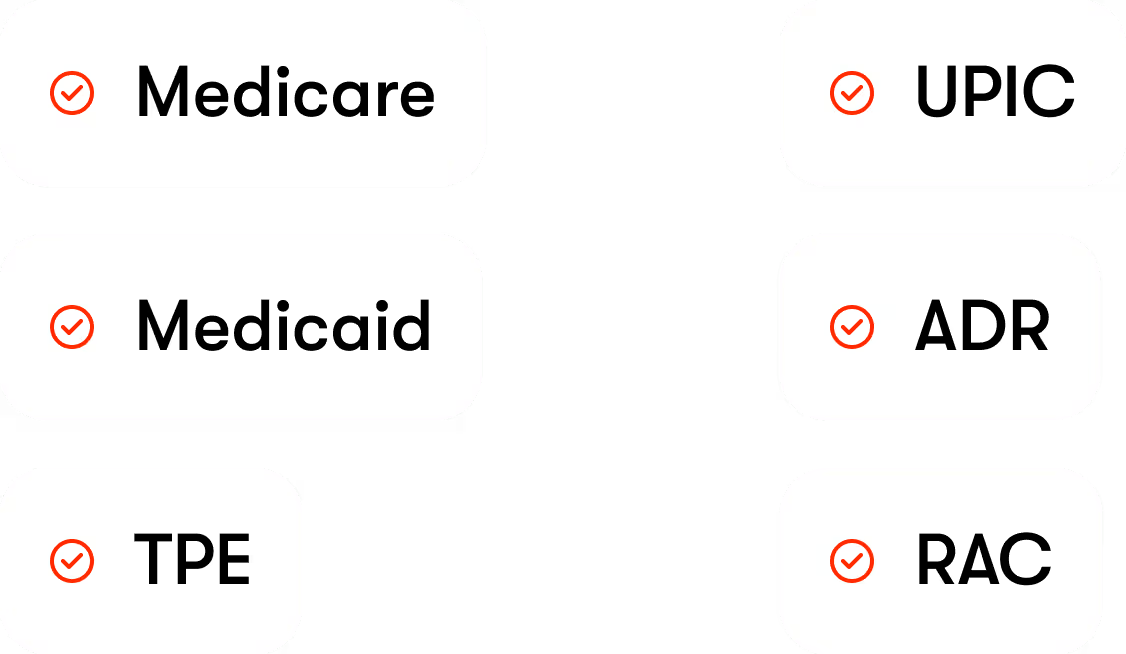
Audits can be intimidating. With Clarity RCM, you don’t need to worry about them. Our team can help you navigate the most complex and daunting regulatory audits, from the notification letter to a successful conclusion. We can handle all Medicare and Medicaid audits, including TPE, UPIC, ADR, and RAC audits.
We’ll lead you through the process and keep you fully informed as we review medical records and collaborate with nurse reviewers, attorneys, payers, and any involved third parties. As an added bonus, we’ll share anything we learn that offers new insight into your practice and how to improve it.